Recruitment Finished!
The FIIX Study has now reached the recruitment target of 730 participants.
The final participants have already been contacted and consented to the study, and will be randomised in the next month.
We appreciate your support in reaching this goal!
Information for Health Professionals
The FIIX Study team would like to acknowledge that the spread of covid-19 across Aotearoa New Zealand may be significantly affecting our participants ability to complete their treatment within the 6 month timeframe.
To mitigate extra stress and uncertainty for our participants and additional strain and stress on your clinics and provision of fertility care, the FIIX study has received ethics approval to increase the primary outcome timeframe from 6 to 7 months and the secondary outcome timeframe from 18 to 20 months for all couples randomised into the study since the 17th August 2021.
We thank you for your ongoing support of this study during such a difficult time.
Welcome!
This page is for health professionals with patients who may be eligible for the FIIX study. You can find useful information and FAQ’s in the boxes below. Click here for the published study protocol.
Who is eligible for the FIIX study?
Couples with unexplained infertility who have been accepted for publicly funded fertility treatment are eligible for the FIIX study.
Couples with mild male factor, mild endometriosis and with at least one patent tube may also be considered. Please see the full inclusion and exclusion criteria below.
Inclusion criteria
1. Eligible for two packages of publicly funded fertility treatment in NZ, which includes all of the following:
a. Age – Female <39 years 4 months and male <54 years and 4 months at the time of randomisation.
b. Body mass index (BMI) – Female – BMI ≤32 (participants who meet all criteria apart from BMI can be discussed on a case-to-case basis with the FIIX team).
c. Both partners are non-smokers for at least three months.
d. Both partners with no history of illicit drug use or alcohol abuse within the preceding 12 months.
e. Day 2 FSH <15IU for the female partner measured in the last 12 months.
f. Both partners must be a NZ citizen or resident, hold a NZ work visa or student visa which allows them to stay in NZ continuously for two years or more, or be an Australian citizen or resident who can prove intention to stay in NZ for two years or more.
g. Couples must have:
i. No previous children from public fertility treatment.
ii. No more than one child (including adopted children) of any age to the same relationship.
iii. No more than one child from a previous relationship living at home (at least half of the time).
2. Female partner has a regular ovulatory cycle (21–35 days).
3. Female partner has evidence of patent fallopian tube(s) on hysterosalpingogram or at laparoscopy or recent intrauterine miscarriage (within 24 months) (tubal spasm is not considered tubal blockage).
4. Male partner has a total motile sperm count (TMSC) > 10 million, on last semen analysis or within two of the past three semen analyses.
Exclusion criteria
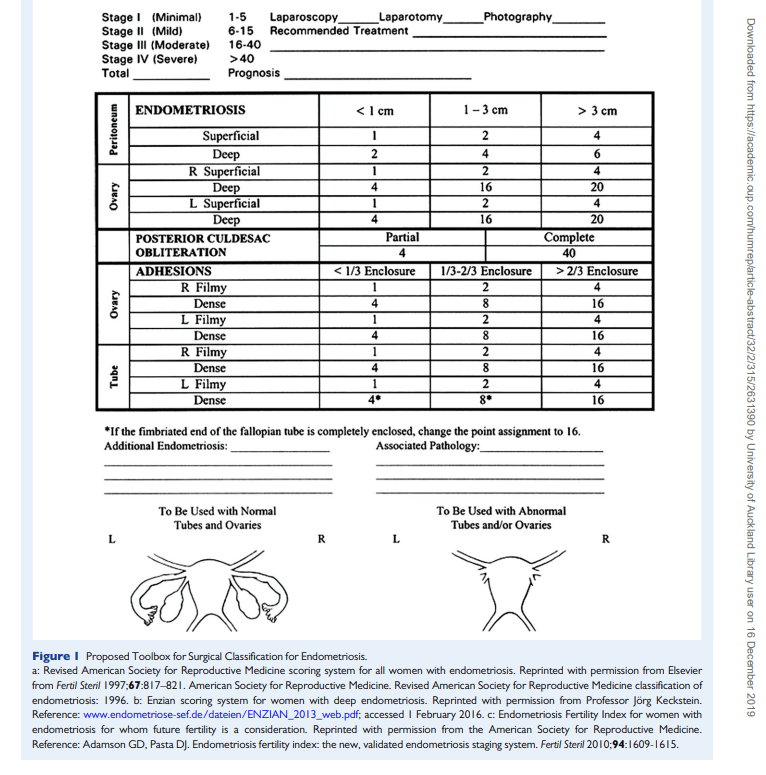
1. Female partner with a history of stage 3 and 4 endometriosis.
2. Female partner with submucosal fibroids or any fibroid >8cm or fibroids between 5-8cm if endometrial cavity is distorted or cavity length is >10cm.
3. Couple who require egg or sperm donation.
4. Female partner with a past history of ectopic pregnancy or bilateral blocked tubes or tubal surgery for adhesions/ hydrosalpinges.
Review of the study inclusion criteria for MAR antibodies and tubal factors
The below revisions have been made in collaboration with clinic staff so the study can better align the inclusion criteria with clinical practice.
MAR antibodies
There is contradictory advice about what percentage of antibodies being positive is considered detrimental to fertility, as such there is currently no standardised reference range. The WHO recommends using the consensus value of 50% motile spermatozoa with adherent particles as a threshold value.1
Previous practice and justification
If over 70% MAR antibodies are present, then the couple are not eligible for the study.
After discussing with a number of both local and international fertility specialists about their own practice and when they would only offer IVF/ICSI we decided 70% seemed reasonable.
Amendment
If over 40% MAR antibodies are present, then the couple are not eligible for the study. However, if the couple are very keen to be included in the study but between 40-70% MAR antibodies are present, the clinic staff and trial team can review their eligibility on a case-by-case basis.
We are now asking for this test to be done for all couples before inclusion in the study occurs.
Justification for amendment
This is the current threshold to score a “6” for male factors on the CPAC form, and is closer to the WHO threshold value.
Tubal factors
We tried to create guidelines to exclude people who clearly had tubal factor while not making the criteria too tight and reducing the number of eligible couples. The study protocol states “Women with a past history of ectopic pregnancy or bilateral blocked tubes or tubal surgery for adhesions/hydrosalpinges are not eligible for the study”.
Previous practice
This is interpreted in clinical practice to mean:
- History of ectopic – not eligible
- Surgically removed tube/s – not eligible
- Hydrosalpinx or tubal adhesions (unilateral or bilateral) – not eligible
- Congenitally absent tube (unilateral) – eligible for inclusion
- Bilateral occluded tubes – not eligible
- Unilateral occluded tube (likely spasm related on HSG) – eligible for inclusion
- Unilateral occluded tube but normal appearance (i.e. not hydrosalpinx) – eligible for inclusion
- Intrauterine miscarriage in past 24 months – eligible for inclusion.
Amendment
Interpreted in clinical practice to mean all of the above (1-6, 8) plus:
7. Unilateral occluded tube but normal appearance (i.e. not hydrosalpinx) – not eligible.
Justification
It is the clinical practice of some specialists not to offer IUI if the dominant follicle is on the same side as the occluded tube due to the risk of ectopic. In other situations (i.e. likely spasm/congenital absence of tube) we feel this is less of a risk, so it is reasonable to consider the couple eligible for inclusion. We want to avoid preventable situations where cycles will be cancelled if the dominant follicle is on the wrong side as this makes it impossible for a participant to complete their IUI package of care (4 complete cycles) within the study’s six-month timeline.
A literature review2 suggests that true unilateral blockage (distal blockage on HSG) has a lower pregnancy rate than bilateral patent tubes. Whereas a proximal tubal blockage – usually reported as likely tubal spasm – has the same pregnancy rate as bilateral patent tubes.
References:
1. Edition F. Examination and processing of human semen. World Health [Internet]. 2010.
2. Tan J, Tannus S, Taskin O, Kan A, Albert AY, Bedaiwy MA. The effect of unilateral tubal block diagnosed by hysterosalpingogram on clinical pregnancy rate in intrauterine insemination cycles: systematic review and meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology. 2019 Jan;126(2):227-35.
What is the TMSC cut-off and how is it calculated?
If the male partner has a total motile sperm count (TMSC) of >10million they are eligible for inclusion in the study. This level can be achieved with mild male factor (i.e. a low count or low motility may still produce a TMSC of >10 million).
Please note the study is using the WHO criteria for TMSC which is volume x count x total motility (progressive + non-progressive). This varies from the TMSC calculated at some clinics and laboratories in NZ which uses volume x count x progressive motility to calculate the TMSC. So the number we get for inclusion may be different to the number reported in the clinic.
The three studies that have compared IUI to IVF for unexplained infertility have used similar thresholds and shown similar live birth rates between the two treatment arms. One study used a threshold of >10million TMSC1, the second used a threshold of >5million TMSC2 and the last study included couples with unexplained infertility (if TMSC >10million) and mild male factor (TMSC 3-10million)3. This is the justification for where we have set our TMSC threshold.
References:
- Bensdorp AJ, et al. Prevention of multiple pregnancies in couples with unexplained or mild male subfertility: randomised controlled trial of in vitro fertilisation with single embryo transfer or in vitro fertilisation in modified natural cycle compared with intrauterine insemination. BMJ 2015;350:g7771.
- Nandi A, Bhide P, Hooper R, Gudi A, Shah A, Khan K, Homburg R. Intrauterine insemination with gonadotropin stimulation or in vitro fertilization for the treatment of unexplained subfertility: a randomized controlled trial Fertility and Sterility 2017: 107, 0015-0282.
- Custers IM, et al. Couples with unexplained subfertility and unfavorable prognosis: a randomized pilot trial comparing the effectiveness of in vitro fertilization with elective single embryo transfer versus intrauterine insemination with controlled ovarian stimulation. Fertility and Sterility 2017, 96(5):1107-1111.
Are couples who have been recommended ICSI due to mild male factor still eligible for inclusion?
There have been some queries raised by clinicians as to whether couples who have been recommended ICSI due to mild male factor can still be eligible for inclusion. As long as the TMSC is >10million, they can. If they get randomised into the IVF arm or require IVF after their four cycles of IUI, then the clinic can determine how the IVF insemination is carried out (either with standard IVF or ICSI).
What happens if the male partner has a bad wash on the day of IUI?
During any fertility treatment the male partner may have variation in semen parameters. For the IUI patients ideally the washed total motile count should be >2million.
If a patient in the IUI arm has a washed total motile count of <2million, please encourage the couple to complete a further IUI cycle, as often these results are sporadic and there is a natural variation in semen parameters from month to month.
It is at the discretion of the clinic team and the couple, whether to proceed with insemination when the washed total motile count is <2million. If the couple chooses not to undergo insemination, this would constitute a cancelled IUI cycle, and the couple is therefore eligible for a further IUI cycle.
If the couple does not wish to have further cycles of IUI, or they have two washed samples with a total motile count of <2million, then they can progress to IVF before completing the 4 IUI cycles, but only after 185 days from randomisation. This wait is to ensure that the study is able to adequately achieve its goal of comparing live birth rate from 4 IUI cycles with one IVF cycle at 185 days (6 months) post randomisation. Couples should be reassured that they will still receive their IVF treatment before they would if they had remained on the wait list. Clinicians should ensure couples understand that they cannot finish their IUI cycles at a later time if they choose to stop their package of care and progress to IVF.
Are patients with a small endometrioma eligible?
If a patient has an endometrioma <3cm with no tubal disease or pelvic endometriosis then they may be eligible. These can be checked on a case by case basis.
If you have any queries or concerns please do contact us at theFIIXstudy@auckland.ac.nz
Approved by Central Health and Disability Ethics Committee on 15 April 2019, reference code 19/CEN/40.